Nigeria clips nurses' wings to prevent brain drain

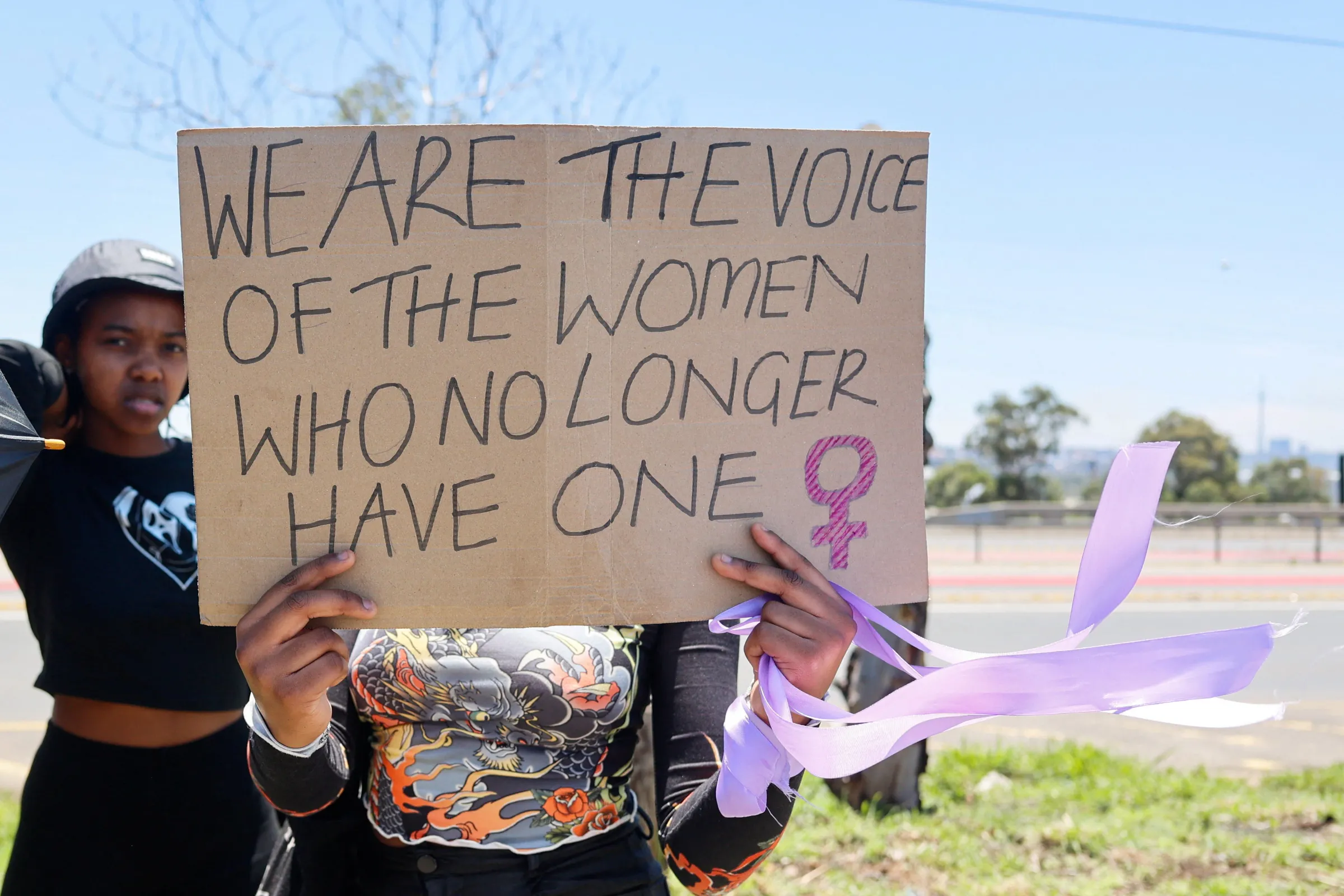
Nurses during a ward round at the University Teaching College Hospital, Ibadan in Nigeria on May 8, 2023. Bukola Adebayo/Thomson Reuters Foundation
What’s the context?
Nurses say government is imposing rules that prevent them chasing a better life overseas
- Healthcare hit as staff opt to work overseas
- Good training and language skills drive the exodus
- New rules slow the nurses' flight
- Advocates say better pay would do more good
LAGOS/MUTARE, Zimbabwe - Nigerian nurse Temitope Ogundare has laid out a fastidious, one-year plan to get himself a well-paid nursing gig in Britain.
Saving half his monthly salary of 45,000 naira ($29) - hard earned in a private clinic - he successfully financed the key English language test needed to bolster his credentials.
Then nailed the required score to get to the next stage of his job hunt.
But now the 25-year-old nurse says his plans are stuck in limbo due to strict, new rules brought in by the Nigeria Nursing and Midwifery Council to ensure home-grown talent stays home.
Like many African, Caribbean and Asian nations with robust education systems and strong English language skills, Nigeria has a brain-drain crisis as an army of nurses, doctors and carers is increasingly drawn to work overseas.
According to its nursing council, about 15,000 nurses left Nigeria last year to take up jobs abroad.
Since 2016, the percentage of African clinical staff working in the National Health Service in Britain has risen from 1.9% to 3.8% in 2023, with most coming from Nigeria.
Stumbling block
The new regulations, which came into force this month, require that applicants to foreign nursing boards clock up two years work experience in Nigeria, and get letters of good standing from a current employer and a past training college.
Applicants must wait at least six months to get the documentation - a process that previously took a week.
The changes sparked protests by nurses who say the rules hold them back and open them to potential abuse from employers.
"This a stumbling block to my career. I am stuck," said Ogundare, a newly graduated nurse.
His current job pays less than $30 a month - income that barely cover his food and journey to work; it doesn't even stretch to his rent.
Nigeria is in the grip of a severe cost-of-living crisis, with consumer inflation running close to 30%, while the local currency has hit record lows and food prices have soared.
Mass exodus
A typical starting salary for a Nigerian nurses ranges from $18 - on a par with the national average - to $50 a month.
Widespread dissatisfaction among health professionals stems not just from the poor pay on offer, but also from the sector's limited career paths and its demanding conditions, leading many to move overseas where they can earn up to 10 times more.
Destinations of choice are Britain, Canada and the United States, countries where entry-level nurses can earn from $36,000 up to $55,000.
Last year, 12,099 Nigerian-trained nurses were registered with Britain's Nursing and Midwifery Council (NMC). Only the Philippines and India surpassed Nigeria as countries with more nurses working in Britain.
But Nigeria says the exodus is hurting its health system, as home-trained nurses head to more affluent countries.
Faruk Abubakar, the registrar of the nursing council - the body that regulates nursing practice - says the new vetting rules are vital if Nigeria is to stem its brain drain.
Abubakar told local media that his council was getting ever more complaints from hospital administrators about nurses quitting without giving due notice, creating scheduling havoc and leaving wards short-staffed.
More than 15,000 Nigerian nurses migrated last year to take overseas employment, he said.
"If we allow every Nigerian to leave as they graduate, who is going to handle our health care services?" Abubakar asked.
He said some of the new rules expressly aimed to protect the nurses, many of whom had to take lower-paying jobs in hospitals and care homes after relocating overseas.
Context reached out to Abubakar for comment on the new rules but received no reply.
Where Zimbabwe leads, Nigeria follows
What awaits nurses in Nigeria has already happened to many of their counterparts in Zimbabwe, which each year loses thousands of trained nurses to Britain and other rich nations.
The Home Office in London said it had issued health and care work visas to 21,130 Zimbabweans in 2023.
Seeking to slow the exit, Zimbabwe's health ministry in 2022 assumed control of the verification process previously run by the country's nursing council, and has since been accused of withholding documents that are crucial to winning foreign work.
Some nurses said they had waited many months for documents that had once taken days to land.
"It is clearly a sabotage plan. They want to frustrate me. I have been waiting for nearly two years," said Precious, 31.
After working five years at the state-run Sally Mugabe Central Hospital in Harare, Precious said she began looking for alternate jobs in Britain to boost her pay.
Most nurses in Zimbabwe earn less than $100 a month and could get at least 10 times that overseas.
Kundai, 38, who works at Chitungwiza Hospital outside the capital, has waited months for her exit documents - with no end yet in sight.
"I tried to follow up recently but was told the papers were not ready. This is so unfair ...," said Kundai, who gave only her first name.
Better pay
As for other ways to stop the brain drain, nursing advocates want governments to give health workers a good reason to stay rather than simply block their exit.
Authorities should provide better pay, offer more opportunities and boost work conditions, said Cynthia Adeyeri from the Nurses Reform Initiative, a Nigerian advocacy group fighting for industry change.
She said a survey of more than a thousand nurses had revealed that some midwives in Nigerian clinics earned as little as 25,000 naira a month - matching the earnings of domestic help and falling below the minimum wage of 30,000 naira.
"If a nurse falls ill, they can't pay for antibiotics from their salary because after they take out transportation (to get to work), there is nothing left to do much," she said.
($1 = 1,560.0100 naira)
(Reporting by Bukola Adebayo; Additional reporting Farai Shawn Matiashe in Mutare, Zimbabwe; Editing by Lyndsay Griffiths.)
Context is powered by the Thomson Reuters Foundation Newsroom.
Our Standards: Thomson Reuters Trust Principles
Tags
- Unemployment
- Pay gaps
- Wealth inequality
- Cost of living
- Migration
- Workers' rights